- It is estimated that 2% to 5% of all patients who undergo surgery will develop a Surgical Site Infection (SSI). These infections are associated with added morbidity, including prolonged hospitalisation by 2 weeks, 5 times the risk of readmission, an increase in average health care costs of up to $26,000 per patient, and twice the risk of death.[1]

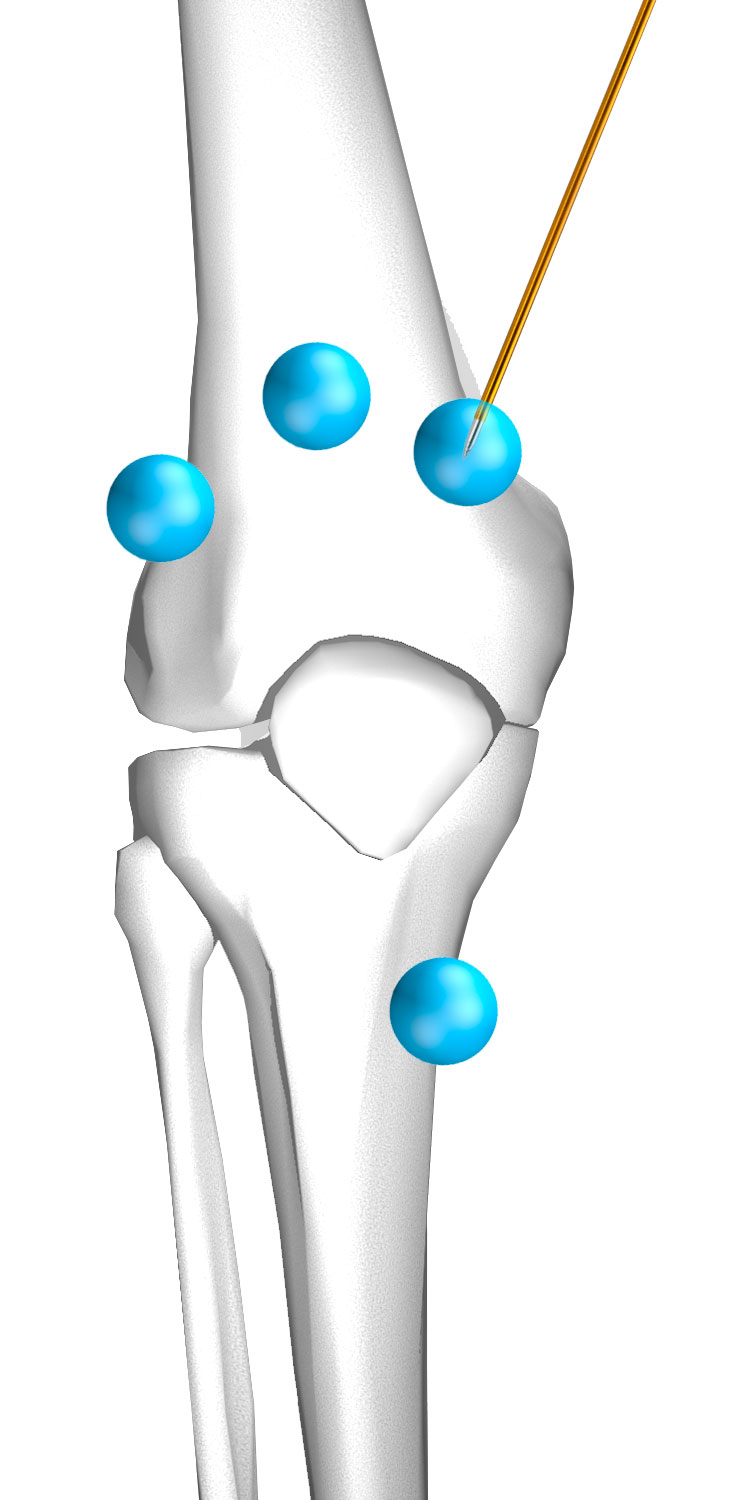
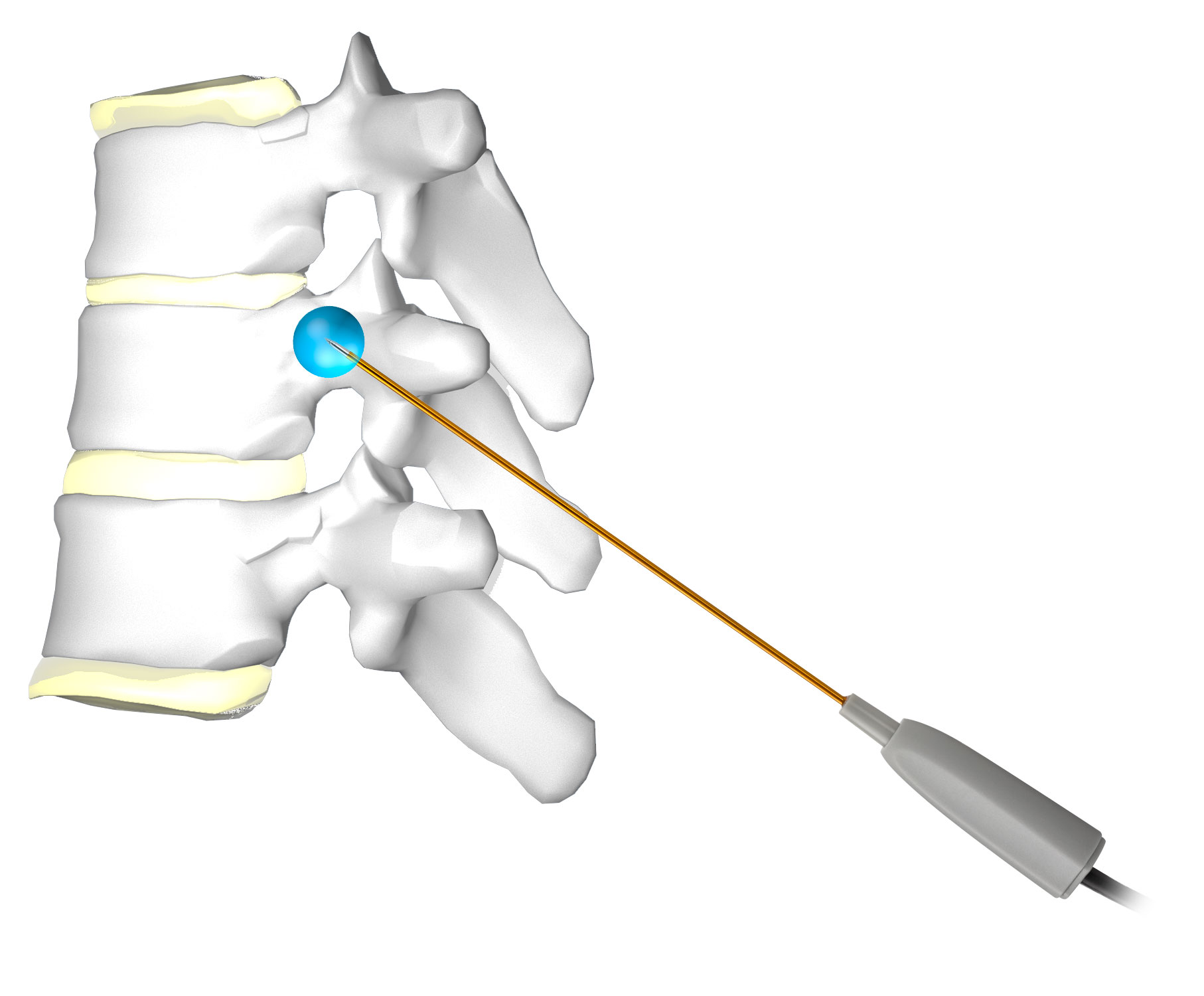
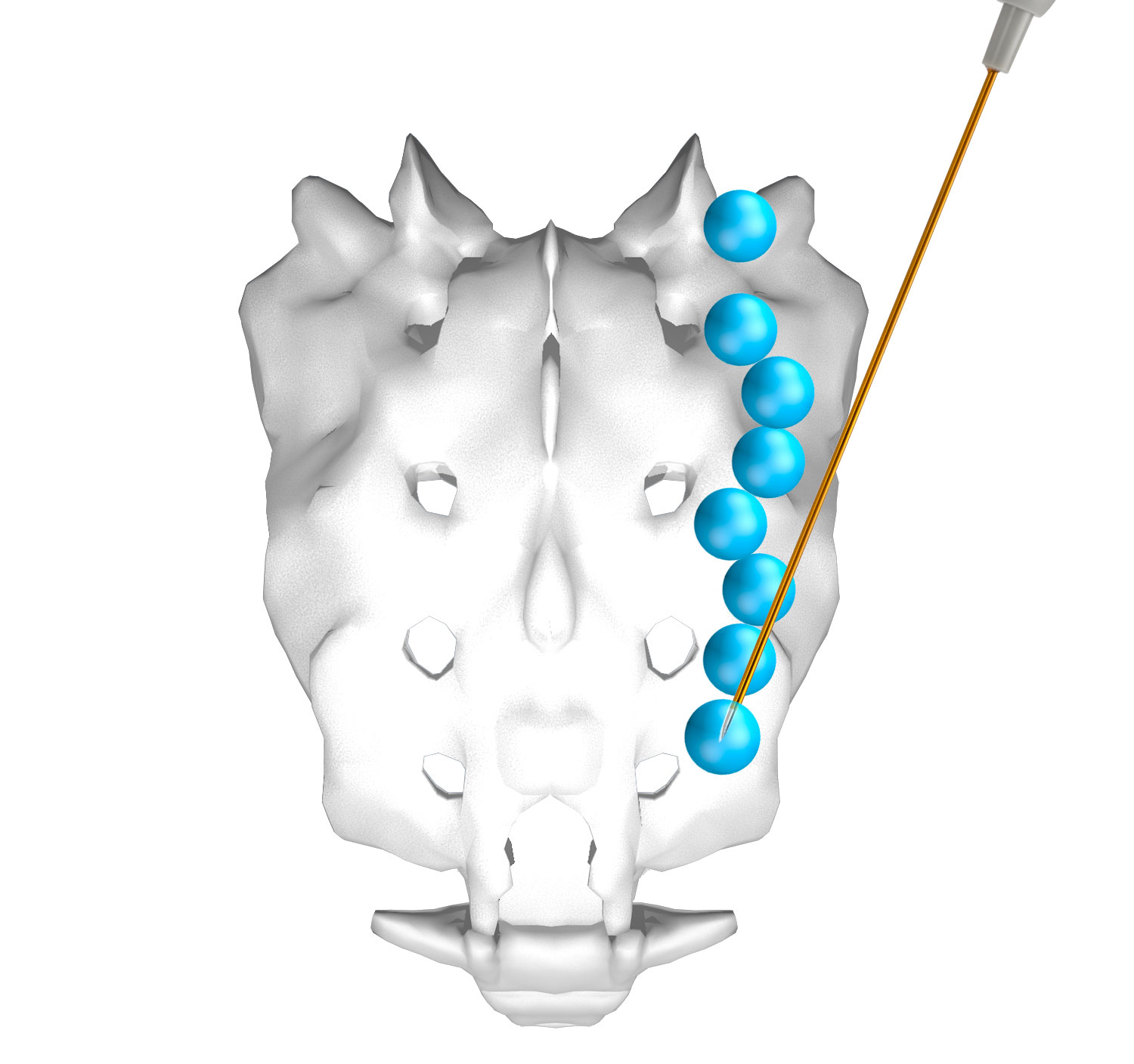
- FloraSeal has been shown to trap and immobilise bacteria that may cause infection to the patient. It rapidly and powerfully kills gram-positive and gram-negative bacteria.[2]
- FloraSeal effectively reduces microbial colonisation within 15 minutes and maintains a low microbial colonisation throughout the 24 hours after application, has the same efficacy when being used with or without an antimicrobial surgical incise drape, and mitigates microorganisms more effectively than an antimicrobial surgical incise drape alone.[3]
1. Towfigh, S., Cheadle, W. G., Lowry, S. F., Malangoni, M. A., & Wilson, S. E. (2008). Significant reduction in incidence of wound contamination by skin flora through use of microbial sealant. Archives of surgery (Chicago, Ill.:1960), 143(9), 885–891.
2. Prince, D., Kohan, K., Solanki, Z., Mastej, J., Prince, D., Varughese, R., & Patel, M. (2017). Immobilization and death of bacteria by Flora Seal microbial sealant. Int J Pharm Sci Invent, 6(6), 45-49.
3. Data on File. Adhezion Biomedical, LLC