- Surgical Site Infections (SSI) have been shown to increase Arthroplasty costs by 61%[1] and it is estimated that 2% to 5% of all patients who undergo surgery will develop a SSI.[2]
- The median cost of treating Prosthetic Joint Infection is $34,800 per patient[3] with infection shown as the cause of 17% of Revision Hips and 24.1% of Revision Knees[4]

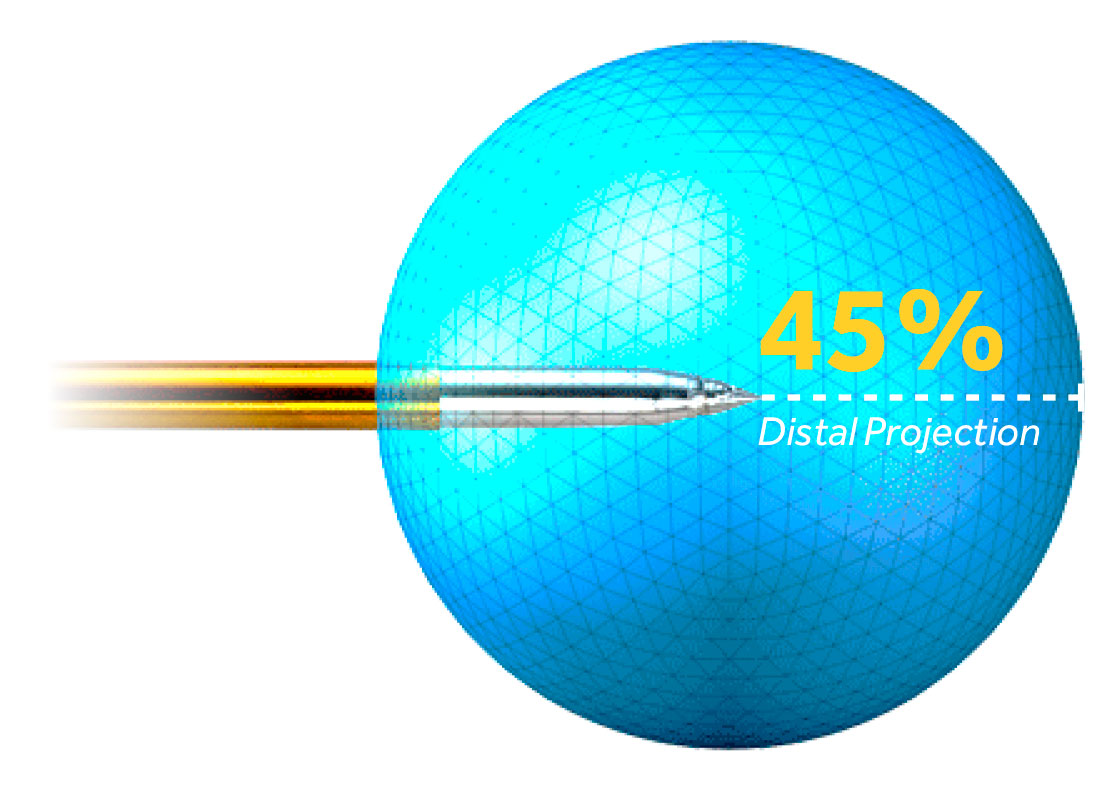
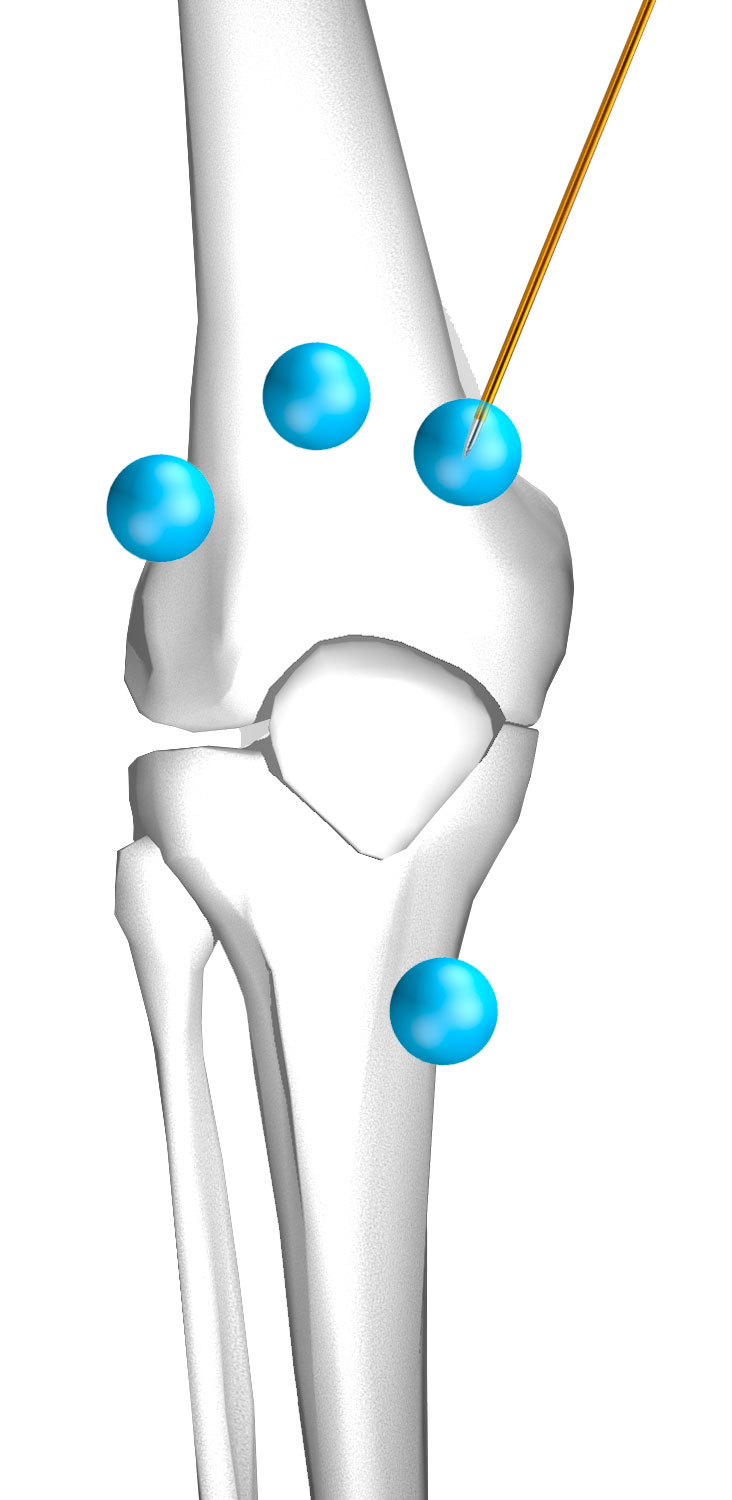
- FloraSeal has been shown to trap and immobilise bacteria that may cause infection to the patient. It rapidly and powerfully kills gram-positive and gram-negative bacteria.[5]
- FloraSeal effectively reduces microbial colonisation within 15 minutes and maintains a low microbial colonisation throughout the 24 hours after application, has the same efficacy when being used with or without an antimicrobial surgical incise drape, and mitigates microorganisms more effectively than an antimicrobial surgical incise drape alone.[6]
1. Peel, T.N., Cheng, A.C., Liew, D., Buising, K.L., Lisik, J., Carroll, K.A., Choong, P.F.M. and Dowsey, M.M. (2015), Direct Hospital Cost Determinants Following Hip and Knee Arthroplasty. Arthritis Care & Research, 67: 782-790. https://doi.org/10.1002/acr.22523
2. Towfigh, S., Cheadle, W. G., Lowry, S. F., Malangoni, M. A., & Wilson, S. E. (2008). Significant reduction in incidence of wound contamination by skin flora through use of microbial sealant. Archives of surgery (Chicago, Ill.:1960), 143(9), 885–891.
3. Peel, T. N., Cheng, A. C., Lorenzo, Y. P., Kong, D. C., Buising, K. L., & Choong, P. F. (2013). Factors influencing the cost of prosthetic joint infection treatment. The Journal of hospital infection, 85(3), 213–219. https://doi.org/10.1016/j.jhin.2013.07.012
5. Prince, D., Kohan, K., Solanki, Z., Mastej, J., Prince, D., Varughese, R., & Patel, M. (2017). Immobilization and death of bacteria by Flora Seal microbial sealant. Int J Pharm Sci Invent, 6(6), 45-49.
6. Data on File. Adhezion Biomedical, LLC